The donor approval process takes several months to complete and involves screening for a range of medical conditions as well as counselling of the donor candidates.
Screening
The screening programme
Our screening method is our raison d'être. It has been at the centre of our operations since we opened in 2004 and we continue to change and update it on a continuous basis. Our screening programme adheres to all national guidelines and EU requirements for screening.

The donor approval process explained
Did you know that only 5-7% of the people who apply to become sperm donors are approved to donate?
In this video, Donor Coordinator Lilian explains our donor approval process to Jo and Viv, an LGBT couple who document their path to parenthood on Instagram.
You'll get the answer to common questions like 'How long does it take to become a donor?' and 'What are the different steps of the donor approval process?'
Before
What are potential donors screened for?
At European Sperm Bank, we screen our donors for the most common serious hereditary illnesses and sexually transmitted infections. We also screen for a selection of other infections on a continuous basis.
Our donors are chosen based on a range of parameters for which they are tested during the screening process:
- The quality and number of sperm cells
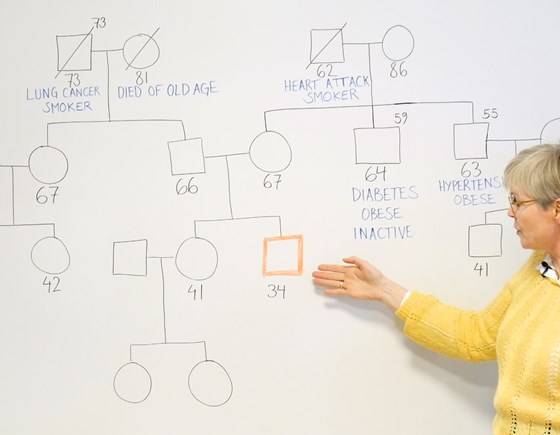
- In order to minimise the risk of the donor being a carrier of e.g. hereditary breast cancer or other dominant hereditary diseases, we carry out a Genetic Risk Assessment based on medical history going back at least three generations.
- Our doctor carries out a thorough physical examination to reduce the risk of the donor transferring hereditary conditions.
- Screening for sexually transmitted infections
- Genetic tests including a chromosome analysis and screening for contagious diseases.
- Personality evaluation
If a donor applicant fails to pass one of the steps listed above, he cannot become a sperm donor.
After
What happens once the sperm donor has been approved?
Once an applicant has been approved as a sperm donor, we continue to test them for contagious diseases. This is done every quarter using a serological test and NAT/NAAT screening.
If we encounter infection of any kind, the sperm donor is quarantined until the disease has been treated. If the sperm donor is infected with hepatitis B, hepatitis C, syphilis, HIV I/II, HTLV I/II, Ebola they will no longer be able to donate.
We determine whether there is new information to respond to with every donation. If, for example, the sperm donor has reported travelling, we will test for any relevant travel-related infections.
When are the donations released?
We adhere to national and international legislation and therefore do not release donations until we have established that the donor did not have any contagious diseases on the donation day in question.
The medical history review
During the screening process, we review the medical history of the donor candidate and his family members.
The purpose of the medical history review is to minimise the risk of a donor passing on a serious condition to children conceived with his sperm.
By speaking to the donor candidate, we collect information about conditions affecting him or his family members. Our Medical Team of clinical geneticists then assess whether a given condition is most likely hereditary or if it is caused by other factors, such as an unhealthy lifestyle (e.g., smoking, poor diet, excessive alcohol consumption).
As part of the review, the donor also needs to pass a physical examination at a specially trained GP.
If our Medical Team conclude that there is an increased risk that children could inherit a serious condition from the donor candidate, we disqualify him.
Want to know more?
If you would like to learn more about the medical history review, you can download a pdf explaining the process in greater detail.
Autosomal recessive diseases
What criteria are considered during the donor candidate screening process?
We do NOT approve applicants with unusual chromosome analyses (karyotypes) and/or who are established as carriers of one or more of the following diseases.
- Cystic fibrosis (CF), mucoviscidosis. The number of disease-causing mutations in cystic fibrosis examined for each donor ranges from 29 mutations to all known mutations depending on when the donor was approved for the programme.
- Spinal muscular atrophy (SMA) was added to the list for all active donors from January 2015.
- Nonsyndromic hearing loss and deafness (DFBN1) was added to the list for all new donors from June 2016.
- Alpha and beta-thalassemia and sickle cell anaemia.
- Tay-Sachs was added to the list for all new donors from July 2019.
In addition, certain genetic tests are conducted for applicants whose family medical history indicates a higher risk of specific conditions:
- Bloom syndrome
- Canavan disease
- Familial dysautonomia
- Fanconi anaemia
- Gaucher's disease
- Mucolipidosis, type IV
- Niemann-Pick disease
- Tay-Sachs disease
The CMV status of our donors
CMV is a common infection that most people get at some point in their lives. We regularly test all our donors to determine their CMV status.
What is CMV?
CMV (Cytomegalovirus) is a herpes virus that is transmitted through saliva or body fluids. It is a common infection that most people get at some point in their lives.
The majority of CMV infections are harmless, and most people do not experience any symptoms. Some people may develop minor symptoms resembling a cold or the flu. In rare cases, CMV can cause health issues for unborn babies.
Once a person has been infected with CMV, the virus remains dormant in the body, but it is not contagious. The virus can be reactivated if the person's immune system is impaired.
The risk of donor sperm transmitting CMV to women or unborn children is extremely low. Even so, we discard donations made by donors with an active CMV infection as a precautionary measure.
Distinguishing between an active and a dormant CMV infection
We regularly test all our donors to determine their CMV status. We do so by screening their blood for the two types of CMV antibodies: IgM and IgG.
When someone becomes infected with CMV, the human body fights the virus by producing IgM and IgG (short for "Immune globulin M" and "Immune globulin G").
What are IgM antibodies? This type of antibodies is present in the blood of someone who has an active (new or re-activated) CMV infection that could infect other people.
If a donor tests positive for IgM antibodies, we discard the donations made during his period of being actively infected with CMV. We are able to do this because we screen donors regularly and don't make donations available for sale until test results come back negative for a range of infectious diseases, among them CMV.
What are IgG antibodies? IgG antibodies are present if a person had a CMV infection at some point in his life. The virus is not active - and thus, not contagious - unless his blood also contains IgM antibodies.
Finding a donor's CMV status
If you would like to know the CMV status of a certain donor, please reach out to us via email, phone or chat. You will find our contact information at the bottom of this page.
Here are the diseases we screen for
Blood sample examination
- HIV I/II
- HTLV I/II
- Hepatitis B
- Hepatitis C
- Syphilis
- CMV
Urine sample examination
- Chlamydia
- Gonorrhea
Depending on the travel history of the sperm donor, we might test for
- Zika
- West Nile Fever
The tests that we perform
ABO - Rh blood typing
The examination reveals the donor's cell count for red blood cells, white blood cells, platelets, and haemoglobin.
The examination reveals the donor's liver function, kidney function, cholesterol, iron level, and blood sugar.
To minimise the risk of the donor being a carrier of e.g. hereditary breast cancer or other dominant hereditary diseases, we go through their medical history going back at least three generations.
Chromosome analyses and screening for the most common serious hereditary diseases with autosomal recessive inheritance.
Thorough physical examination by our doctor in order to minimise the risk of the donor transferring a hereditary condition.
Screening for sexually transmitted infections. We screen for other infections through blood or urine samples on a regular basis.
Screening your genes
Rule out the risk of 400+ diseases
We screen our donors well, but if you're the birthing parent, your genes also affect your child's health. By screening your genes for hereditary disease with GeneXmatch, you'll gain greater peace of mind.
